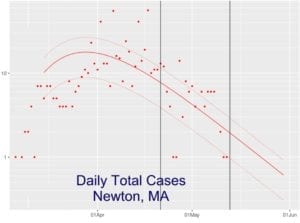
 In a recent open-thread comment, data wrangler Jack Prior announced that he has added Newton data to his remarkable COVID-19 forecasting model of cases, hospitalizations, and deaths. But in his comment he neglected to include key findings from his analysis, some of which are outlined his COVID-19 analysis blog post.
In a recent open-thread comment, data wrangler Jack Prior announced that he has added Newton data to his remarkable COVID-19 forecasting model of cases, hospitalizations, and deaths. But in his comment he neglected to include key findings from his analysis, some of which are outlined his COVID-19 analysis blog post.
His findings are good news for Newton:
- Newton is already largely through its infection period and 10 days from now may start to average less than 1 new case per day.
- Newton has had 675 cases and is forecast to have another 25.
- Newton has been steadily slowing its growth rate of cases by 9% per day, which is significantly better than Massachusetts’ case growth, which is slowing by 5.9% per day. Newton’s case growth is better than all states except Montana and Hawaii.
- Newton’s case growth is approaching 0.1%, which was the rate China and South Korea reached when nearly eradicating the virus.
Jack Prior’s forecasting model has lots of dials and sliders to let you select particular geographical regions, time periods, data series, scales, etc. for your own analysis. It constantly grabs the latest data from various sources described in this page of notes, caveats, and source citations.
This is great work by Jack. Tip of the cap and a thank you.
I really appreciate Jack’s visualizations but am less comfortable with the modeling, or any models that don’t incorporate parameters from infectious disease epidemiology. It’s also important to remember that as soon as controls are lifted, case numbers soar (as is currently happening in South Korea, for example).
As long as only a relatively small proportion of the population has had COVID-19, we have to be very careful that we don’t open up too quickly and start filling the hospitals again. That’s why a staged plan like the one set out by Governor Baker is so important. This is going to be a long haul, at the very least until we have effective treatments or a safe effective vaccine.
Hi Meridith — Yes, the extrapolation model can only predict what will happen if nothing changes on the ground. On the other hand, it can detect when changes on the ground happen with objective sensitivity (see Alabam) as well as convey how far there is to go to get to a level where control removal can be contemplated.
If Newton were an island, we would be getting close. Unfortunately, we are not. Massachusetts has a ways to go, but we have the potential to get to very low levels with a bit more patience or careful staging.
Looking back through final projections using this method they ranged from 600-800 over a month ago, so we have stayed on our trajectory. The big variable has been step discoveries/disclosures of unreported nursing home infections and delayed test result batches.
@Meredith, I agree with your major point that our return to normal life will lead to new waves of COVID-19. But epidemiological models can be wrong as well. The most such model, from the University of Washington, was wildly optimistic when it mattered most, and was thus used by POTUS to gaslight us.
Also, South Korea’s 2nd wave has thus far been pretty minimal, I think because they do such a good job of testing and contact tracing:
https://www.worldometers.info/coronavirus/country/south-korea/
@John White – I never said that epidemiologic models are always right! My motto, right at the top of my blog, is statistician George Box’s maxim that all models are wrong but some are useful.
If you are referring to the IHME model, it’s not an epidemiologic model – it’s a statistical model. Two very different creatures. Lots of discussion on epitwitter complaining about it.
And epidemiologists will be the first to say that their models will become outdated as situations change. That’s why the best papers have shown a range of models specifying the reasons they differ (for example, a graph with physical distancing, a graph with no controls, etc.)
@Meredith — No offense or attack toward you or the modelers intended. I like differential-equation-based models as well, because they give us a decent idea of what parameters we need to adjust to bend the trajectories, and because we have great tools to understand their generic behaviors. I also like the graphical approach @Jack Prior has taken. One can learn a lot about the near future by noting when doubling times change.
Forecasts aside, it appears that with other hot spots further down the curve, and others not having risen yet, that MA currently has the highest per capita death rate in the world…
https://jackprior.shinyapps.io/covid19code/?_inputs_&look=%222020-07-01%22&sdw=%5B%222020-04-23%22%2C%222020-05-13%22%5D&aspect=%22Daily%22®ion2=%22_USA%22&scope=%22USA%22&feature=%22Deaths%22&state=%22MA%22&log=false&mode=%22Rank%2FPop%22®ion=%22_World%22&country=%22_France%22&country2=%22_USA%22&state2=%22NY%22
@Jack Prior. Many thanks for sharing this information. You really are Newton’s latter day Paul Revere.
For those who are still not wearing masks or social distancing (you know who you are, don’t make me come up there).
Imagine you have no symptoms, but you are infected with the virus. Every time you go out in public without a mask, or fail to follow the CDC guidelines about social distancing, you are putting someone at risk. Maybe a stranger, or maybe a grandparent, parent, sibling, close relative, friend, or significant other.
Don’t be a Covidiot. Wear. A. Damn. Mask.
That is all.
@John – I didn’t take it as an attack. I like differential equations, too – a lot of infectious disease epidemiology models use differential equations. The part I like to see is incorporating parameters like R0 and seeing what happens when they vary.
@Jack – I’m a statistician working on HIV clinical trials and understand that different approaches have different uses. What you say about your model being good for detecting changes makes sense. From what you say, I gather it’s meant as a descriptive model more than a predictive one – is that correct?
It’s appalling that deaths in group homes comprise such a huge proportion of the total. Sadly, after having been in one last year for 2 weeks of rehab, I’m not surprised – many of the aides were careless about hygiene (whether through overwork or inadequate education and supervision or both). There was a good opinion piece recently on the part played by having wages so low that the attendants need two jobs to survive, which means they are bringing viruses from one place to another, especially since many of them are hourly with little or no paid sick leave.
Cool, looks like time to open.
@Ted, since you presumably are not entering the homes of strangers at present, you must be referring to people not wearing masks outside.
There is simply no need to wear a mask when jogging or walking the dog if you don’t come within 6′ of another person. And I assure that nobody on the mean streets of Newton will come that close to another person.
Pretending that wearing masks in solitary outdoor activities does anything to stop the spread of this virus is not accurate.
@Meredith — I would say the app is descriptive and near-term predictive. If behaviors don’t change, it is pretty good at predicting how things play out; even over several weeks. For the US, the key is that things are improving later and more slowly than in EU and Asia. Once behavior changes, it can adapt to that new behavior with a couple weeks of data collected.
It is not “prescriptive”, as it doesn’t anticipate or model scenarios of behavior and their impact. That is where more advanced models come into play.
@Craig — with outdoor gusting winds 6ft becomes 15+, so it is just common courtesy to have a mask at the ready if you are outdoors, and to put it on if you are within 25 ft of others.
Many people are going to great lengths to protect their loved ones with social distancing. The risk of person-to-person transmission outdoors may be very low, but for many it feels like the highest risk they are taking right now. I run with a technical gaiter that is easy to raise up or down during a run and also easy to wash.
Let’s just remember that some people can’t wear masks. Both the state and city have set forth that those who can’t wear masks are exempted and are not required to provide proof of the reasons they can’t wear masks.
So please let’s all wear masks if we’re able to but refrain from vitriol if we see someone not wearing one.
@Jack Prior: You claim that in the presence of wind gusts, there is a meaningful risk that contagious amounts of coronavirus will be carried from a person’s breath over 25 feet. You use this argument to admonish the public that they need to wear masks within 25 feet of each other.
Would you please show us how you calculated this?
From the little I know about fluid dynamics, I disagree with you. Because of entropy, wind disperses airborne particles over a greater volume of space. (Everyone intuitively knows this from watching smoke from a chimney).
What does that mean? In almost all cases, wind will REDUCE the likelihood that a passerby will contact an airborne particle from a nearby person. It also reduces the median dose that a passerby will receive. Both of those phenomena reduce the risk of transmission.
The faster the windspeed, the more dispersion. Dispersion is even greater if the airflow is turbulent, which is often the case with gusty winds.
You don’t have to take my word for it. See what the Harvard School of Public Health has to say: https://www.hsph.harvard.edu/news/hsph-in-the-news/is-it-ok-to-play-frisbee-during-social-distancing/
This is not just an academic debate. First of all, you are well respected on this site as a statistician. People are going to take what you say seriously. If you are going to tell strangers how to behave, you ought to provide solid reasoning.
@Michael — fluid dynamics: https://covid19.jackprior.org/2020/04/06/running-and-covid-19/
Someone who is exercising is projecting their airflow more vigorously than normal, potentially with more aerosols than normal, like choir singers:
https://www.christianpost.com/news/86-percent-of-choir-members-got-infected-covid-19-church-practice-washington-report.html
Weak science aside, I’m really just making an emotional pitch — more than a scientific one — for common courtesy. There is no risk at 25 ft. There is probably no risk at 15ft. After that, why stress each other out? Pop your mask on while near folks. Plenty of people are getting sick trying to do all the right things. Until actual common modes of transmission are very well understood, err on the safe side for others.
@Jack Prior: Thank you for clarifying that your 25-foot guideline was an emotional pitch. The problem is that 25 feet is arbitrary. Why not 100 feet? Why not a mile?
When the public sees smart people like you declare that wind can transmit the virus between people who are 25 feet apart, they worry that virus can be carried in building HVAC ducts or between passing cars. As you say: why stress each other out?
I know you have the best of intentions. You are clearly a very talented scientist. Keep serving up what you do best–scientific reasoning!
@Micheal — You asked for a scientific basis for risk of outdoor spread based on fluid dynamics, I gave you a scientific basis in fluid dynamics (https://play.vidyard.com/ThymLoySe295KXmCmJJd57). One that I posted weeks ago and the basis for my statements.
I’m suggesting that if you are 25 feet away from folks, don’t worry about it, but don’t wait until you are 12 feet away or 6 ft away to put on a mask, or disregard the risk entirely. If you don’t buy into the risk, at least emotionally recognize the offensiveness of the behavior to those that do.
@Jack thank you for your work and sharing it in such a detailed manner. I’ve been a frequent flyer to you site! However, you are wrong about the outdoor transmission. All the detailed infection tracing has shown quite clearly that outdoor COVID transmission is extremely rare and the few cases identified have been stationary conversations between unmasked individuals. Six feet distance with a mask is a safe combination when outside. A shallow dive on this subject can be found here in a Times article
What We Know About Your Chances of Catching the Virus Outdoors
Wind is actually beneficial – dispersing and reducing the virus load.
https://www.nytimes.com/2020/05/15/us/coronavirus-what-to-do-outside.html
@Peter — Yes, today’s NYT article that you linked to provides some assurance on the matter. Still, I would maintain the 6ft bubble shifts a bit with wind and motion (particularly for a cough or sneeze). I’d also maintain the absence of evidence is not evidence of absence in terms of actual transmission. Many cases are not traced folks have no idea how they got it.
I would agree that 6 feet with two masks outside is likely fine. The debate seems to be around whether 7ft requires no masks outdoors, or whether they are needed at all.
If you are in motion toward someone moving rapidly, and you are not wearing a mask, the other party is not in control of keeping the 6ft distance, so it can create justified anxiety on their part.
So I’m propose leaving some extra room for a wind shifted bubble, and having the courtesy to have your mask well before you approach that bubble, rather than fumbling to put it on at the last moment. To me, that’s about 25 feet.
Here is the academic paper associated with the video above:
http://www.urbanphysics.net/Social%20Distancing%20v20_White_Paper.pdf
“This suggests that avoiding substantial droplet exposure in the conditions of this study and in a way equivalent to the 1.5 m for people standing still can be achieved by one of two actions: either by avoiding to walk or run in the slipstream of the leading person and keeping the 1.5 m distance in staggered or side by side arrangement, or by KEEPING LARGER SOCIAL DISTANCES, where the distances increase with the walking or running speed.”
For the record, I’m a chemical engineer by training, rather than a statistician…
Getting back to the app — it now has testing information, showing the trends in testing done in each state as well as how states rank against each other. http://app.jackprior.org
@Jack – thanks for posting the link to the White Paper, confirming what is demonstrated in the video, as well as all your data, modeling and tracking!
Here’s a really excellent 4-minute video by Professor De Kai on how masks can help turn the tide of infection in a community: https://youtu.be/yfeW2l8G_W4
I was able to add a new metric to the app that estimates the extent a state has proceeded through its infection cycle that could be a means to assess reopening readiness. It is explained in this blog post:
https://covid19.jackprior.org/2020/05/17/metrics-for-reopening-readiness/
Would appreciate opinions.
I really don’t know why anyone is quibbling with Jack over distances and when and when not to wear a mask. Beyond his technical prowess, he’s just advising folks to take the worst case scenario to protect themselves and others. We may be able to modify these distances as more information about this data is fully established, but why take chances if there’s even the hint of a chance that the virus is as deadly as Jack concludes it may be. What is the big deal with me pulling my mask up in public when someone gets within 25 feet of me. Jack mentioned “emotional” considerations. I will get very emotional if some clown comes close to be without a mask and proceeds to cough or sneeze. Wear the mask, damn it.